The new Ontario HIV Epidemiology and Surveillance Initiative (OHESI) report – “HIV diagnoses in Ontario, 2019” – describes trends in HIV diagnoses in Ontario over the past decade (2010-2019) with a focus on first-time HIV diagnoses in 2019. It includes overall findings as well as trends among Ontario’s five priority populations (i.e. subgroups of Ontarians who experience a higher risk of HIV), broken down sex, HIV exposure category, race/ethnicity, age, and geographic location.
Some key findings from the 2019 Diagnosis Report
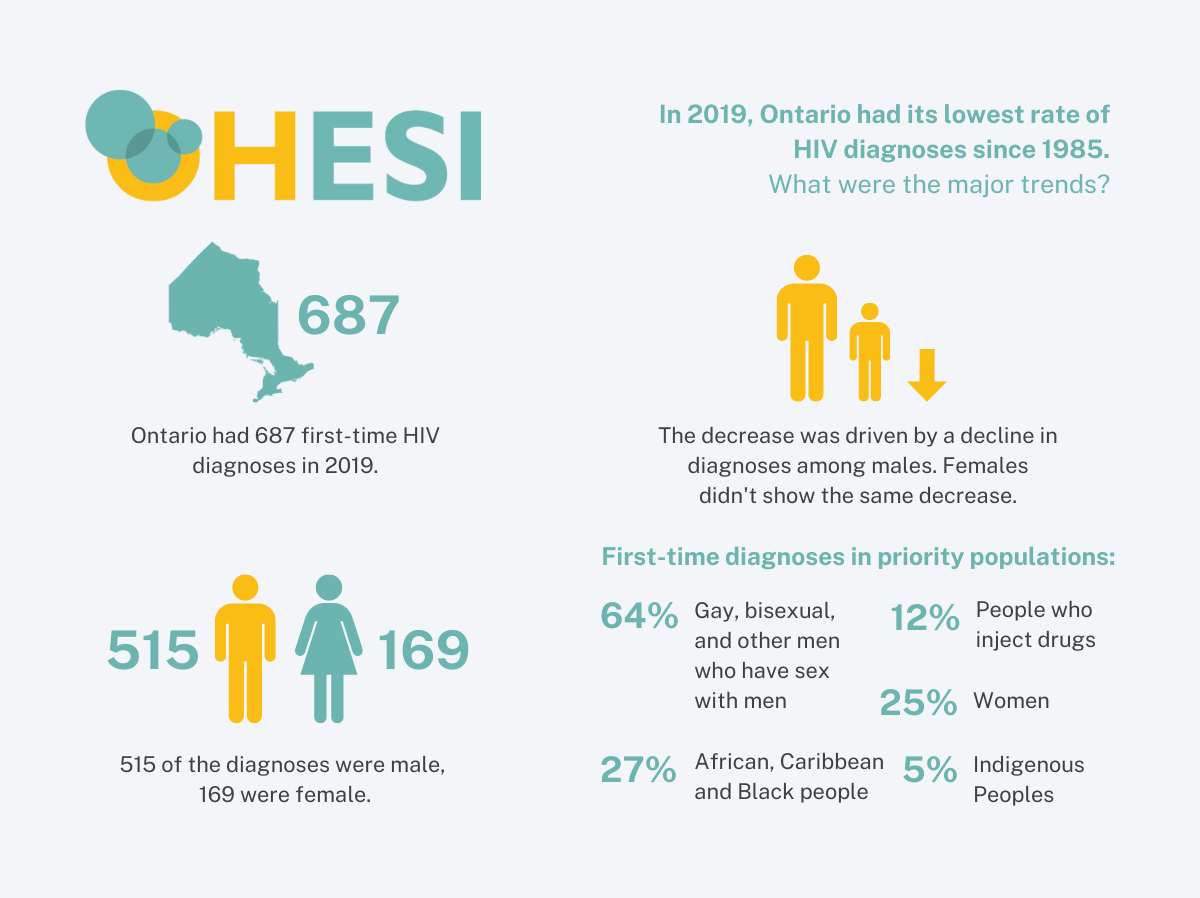
2019 had the lowest rate of HIV diagnoses since 1985
In 2019, the number of first-time HIV diagnoses was the third lowest it has been since 1985 (when Ontario first started testing for HIV). Relative to the population size, the rate of HIV diagnoses per capita in 2019 was the lowest it has been since 1985.
Ontario reports surveillance data for the number of first-time HIV diagnoses annually (our best indicator of the number of people who are learning their HIV status for the first time and were likely to have been infected in the province), as well as people with previous evidence of HIV who are entering care in Ontario (including people who have migrated to Ontario and already knew their status). Due to missing data on HIV test history, we estimate between 6.3% and 7.5% of first-time HIV diagnoses overall to have an uncaptured previous HIV diagnosis.

Decreased rate driven by decline in diagnoses among males
In 2019, Ontario saw the lowest number of first-time HIV diagnoses in males since 1985, as well as the lowest rate per capita.
The number and rate of first-time HIV diagnoses in females has not seen the same decrease as in males, remaining fairly consistent over the past ten years.

Diagnoses decreased in white males but not in racialized males
Throughout the epidemic, white males have accounted for the largest numbers of first-time HIV diagnoses. However, while still representing the largest numbers, the number of white males diagnosed with HIV for the first time has decreased in recent years – a trend not seen in males of other races/ethnicities. On the contrary, the number of Latin American males diagnosed with HIV for the first time has increased in recent years.

Male-to-male sexual contact remains the predominant HIV exposure category
For the first time, this report describes breakdowns of first-time HIV diagnoses by HIV exposure categories: these are mutually exclusive categories (assigned by hierarchy) meant to represent an individual’s most likely means of HIV acquisition.
In 2019, among the 480 first-time HIV diagnoses with a reported HIV exposure category, a majority (59.2%) reported male-to-male sexual contact, and this has been stable over time.
Considerably fewer diagnoses reported heterosexual contact with identified risk (15.2%), heterosexual contact with no identified risk (12.5%), and injection drug use (IDU, 8.1%).

Note: The “Heterosexual contact, identified risk” category includes diagnoses where sex with a person of the opposite sex/gender is reported and either the individual’s country of birth is reported as an HIV-endemic country, or the individual’s sex partner is reported to be at least one of: HIV-positive; user of injection drugs; born in an HIV-endemic country; a bisexual male.
Priority populations
Gay, bisexual, and other men who have sex with men (GBMSM) continue to account for more than 6 out of 10 diagnoses
HIV is not a generalized epidemic in Ontario. It is concentrated in a small number of populations that have higher HIV prevalence than the general population: known as “priority populations” for HIV programming in Ontario’s response to HIV. Priority populations are not mutually exclusive: a person can be a member of multiple priority populations.
In 2019, among the first-time HIV diagnoses where reported information was adequate to assign a priority population, nearly two thirds of first-time HIV diagnoses were attributed to GBMSM, followed by just over a quarter of first-time HIV diagnosis attributed to ACB.

Priority populations: Take Away Messages
- The number of first-time HIV diagnoses among gay, bisexual and other men who have sex with men (GBMSM) decreased from 343 in 2018 to 307 in 2019, driven largely by decreased diagnoses in white GBMSM, likely due to HIV pre-exposure prophylaxis (PrEP) uptake in that population.
- More African, Caribbean, or Black (ACB) males were diagnosed with HIV in 2019 than ACB females: a trend that has been consistent for as long as the surveillance data has been able to define ACB people (since 2009). Nearly two thirds of these ACB males reported their HIV exposure category as male-to-male sexual contact.
- The majority of people who use injection drugs (PWID) diagnosed with HIV throughout the epidemic have been male. Between 2016 and 2019, the South West region saw a steady 73% decline in first-time HIV diagnoses among PWID.
- While more Indigenous people were diagnosed with HIV in the Northern region than in any other health region in 2019, 59.3% of first-time HIV diagnoses in Indigenous Peoples were outside the north, principally in South West, Toronto, and Central West regions.
- When HIV exposure category was reported, half of Women diagnosed with HIV for the first time reported an exposure of heterosexual contact with identified risk[1] (53.7%), while a quarter reported heterosexual contact with no identified risk1 (23.2%) and a quarter reported injection drug use (23.2%).
Much more information is included in the report, available here.
Supplementary tables are available here.
Stay tuned for more OHESI reports coming soon!
OHESI is a collaboration involving AIDS and Hepatitis C Programs of the Ontario Ministry of Health, Public Health Ontario, the Public Health Agency of Canada, and the Ontario HIV Treatment Network. The objectives of OHESI are to analyze, monitor and disseminate knowledge products on the epidemiology of HIV in Ontario.
[1] The “Heterosexual contact, identified risk” category includes diagnoses where sex with a person of the opposite sex/gender is reported and either the individual’s country of birth is reported as an HIV-endemic country, or the individual’s sex partner is reported to be at least one of: HIV-positive; user of injection drugs; born in an HIV-endemic country; a bisexual male.