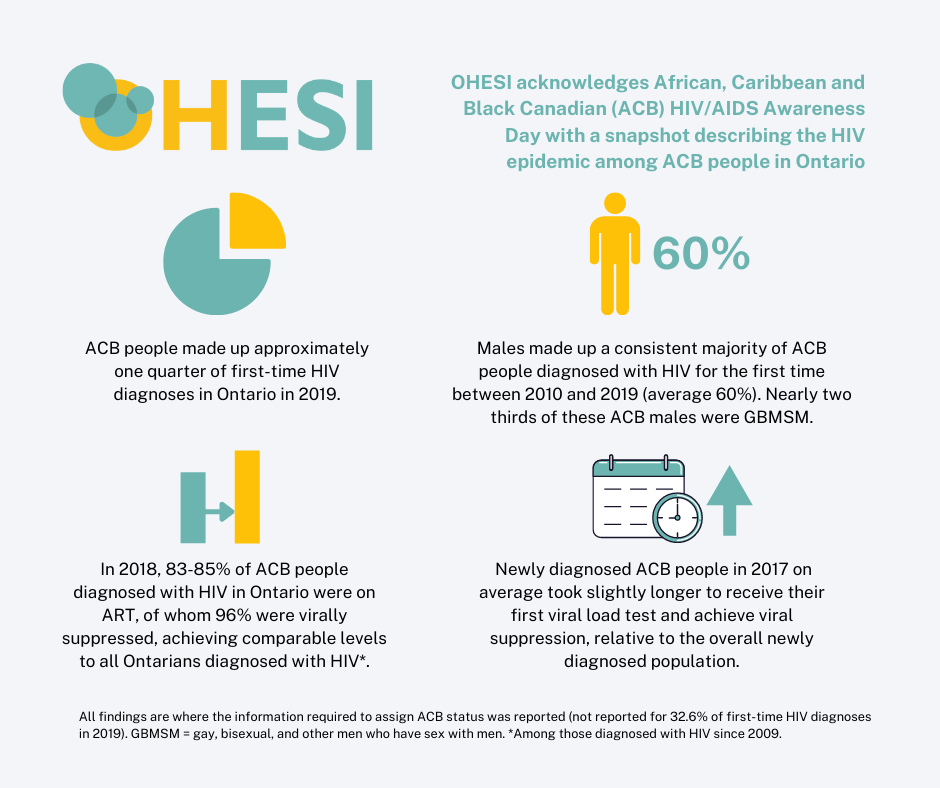
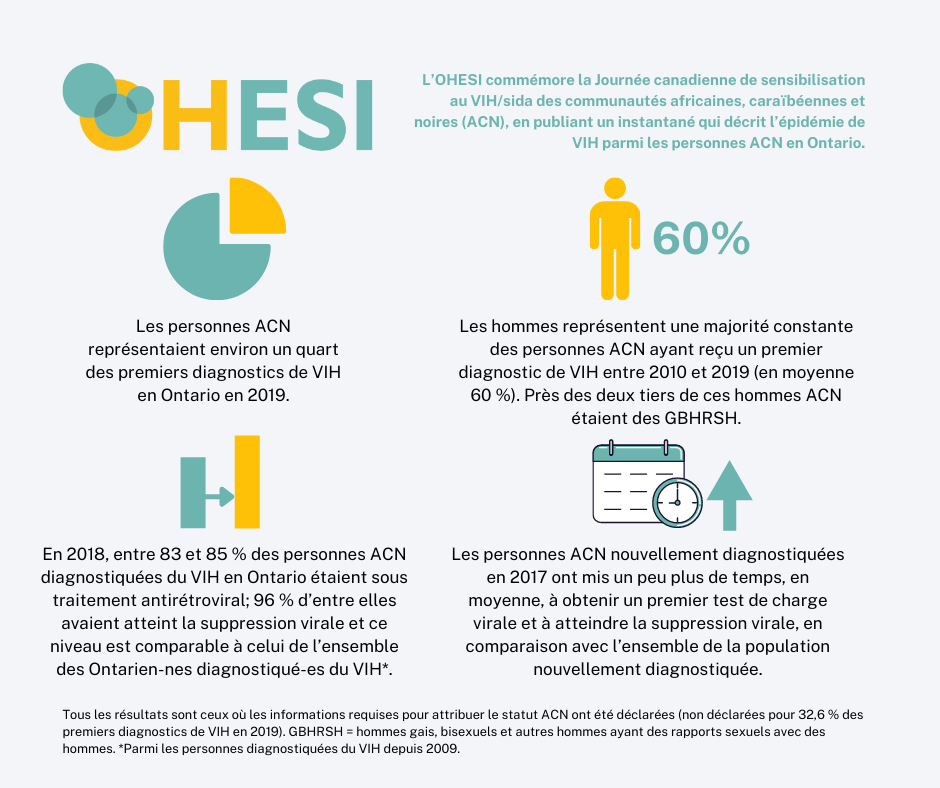
To commemorate African, Caribbean and Black Canadian HIV/AIDS Awareness Day on February 7, 2022, the Ontario HIV Epidemiology and Surveillance Initiative (OHESI) is pleased to provide a snapshot describing the HIV epidemic among African, Caribbean, and Black (ACB) people in Ontario – one of five priority populations (subgroups of Ontarians who experience a higher risk of HIV). This blog post highlights findings from our recently released report, “HIV diagnoses in Ontario, 2019”, as well as new indicators on the proportion of ACB people diagnosed with HIV who are in care, on treatment, and virally suppressed. Although ACB people continue to bear a disproportionate burden of HIV, those diagnosed with HIV in Ontario are largely engaged in care and virally suppressed. When ACB people are diagnosed, they achieve health outcomes comparable to all people diagnosed with HIV in the province.
Key messages:
- Members of the African, Caribbean and Black community who are diagnosed with HIV in Ontario fall into two distinct groups:
- People diagnosed for the first time in Ontario who are more likely to have acquired HIV here.
- People living with HIV who were diagnosed elsewhere (i.e. have previous evidence of HIV) and moved to Ontario (mainly from countries in Africa or the Caribbean with a higher prevalence of HIV in heterosexual populations).
- It’s important to understand the nature of both these groups to:
- plan the right mix of care, treatment and other services for those who already know their status as well as those who are newly diagnosed, and
- understand who is at risk of HIV acquisition and use that information to strengthen prevention programs and testing programs to diagnosis ACB people living with HIV.
- At least 45% of the 229 ACB people overall (~53% of ACB females in particular) who received a positive HIV test in 2019 already knew their HIV status (had previous evidence of HIV) and were entering care in Ontario for the first time, while as many as 55% were first-time HIV diagnoses. Of the 104 ACB people with previous evidence of HIV, 63 were female and 41 were male. It is important to note that, when information on test history is missing, individuals are categorized as first-time HIV diagnoses by default and that, therefore, these figures likely overstate the proportion classified as first-time HIV diagnoses. OHESI estimates approximately 10% of ACB people classified as first-time HIV diagnoses had prior knowledge of their HIV status.
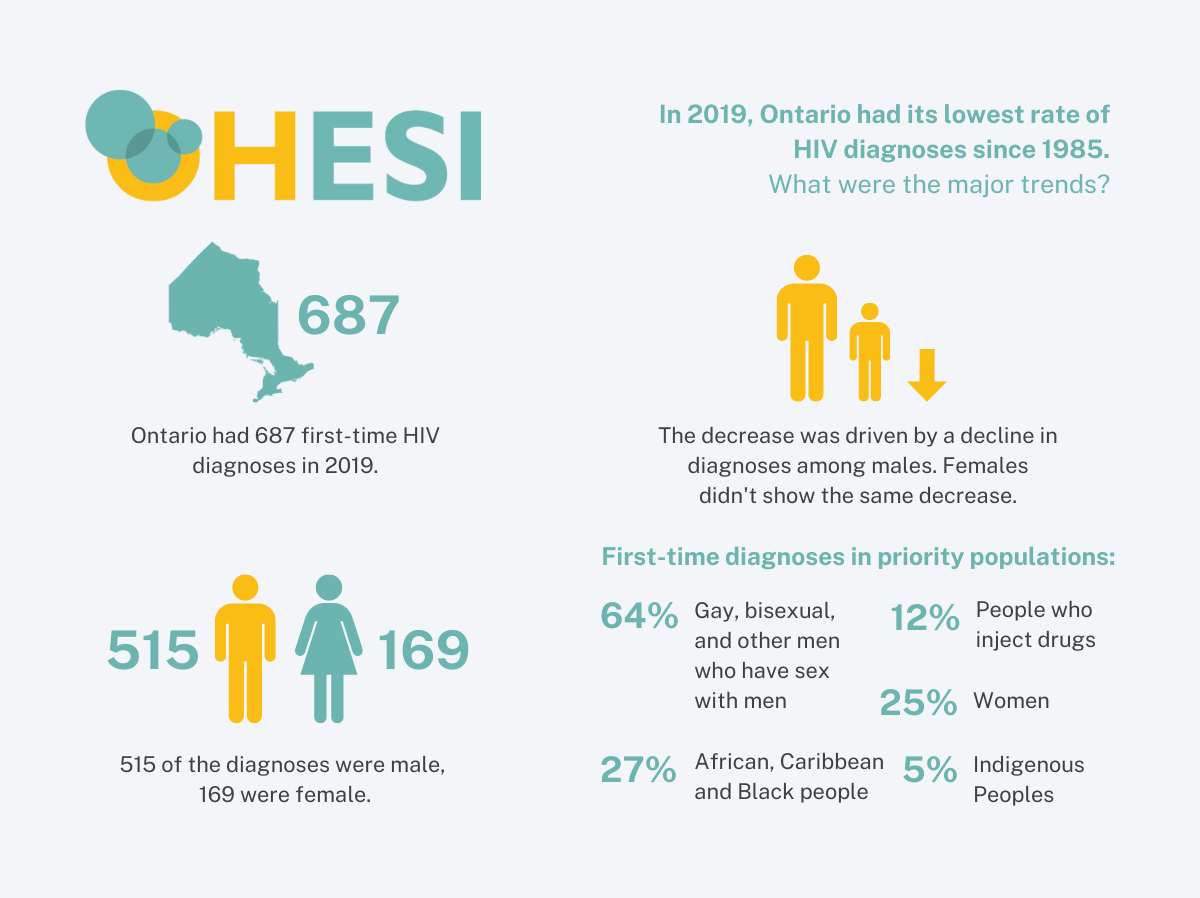
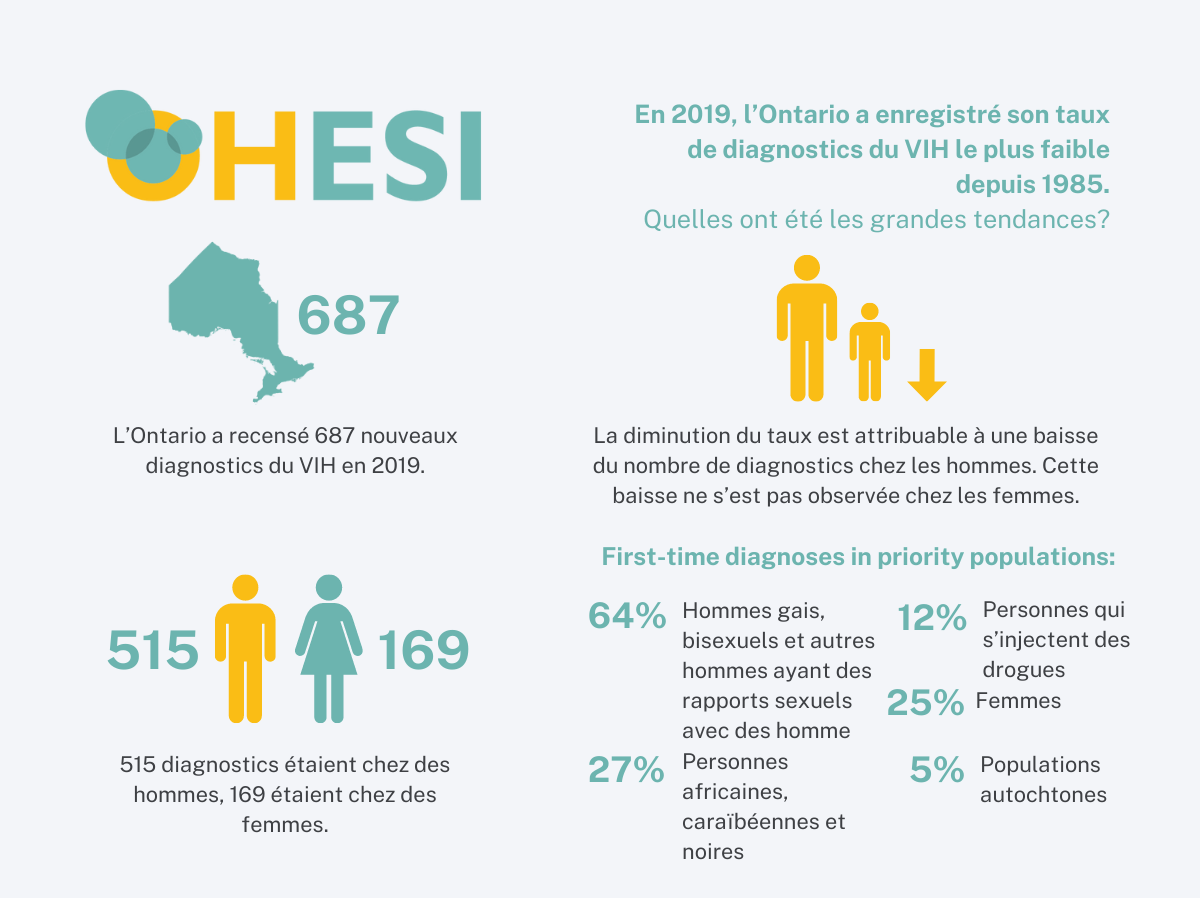
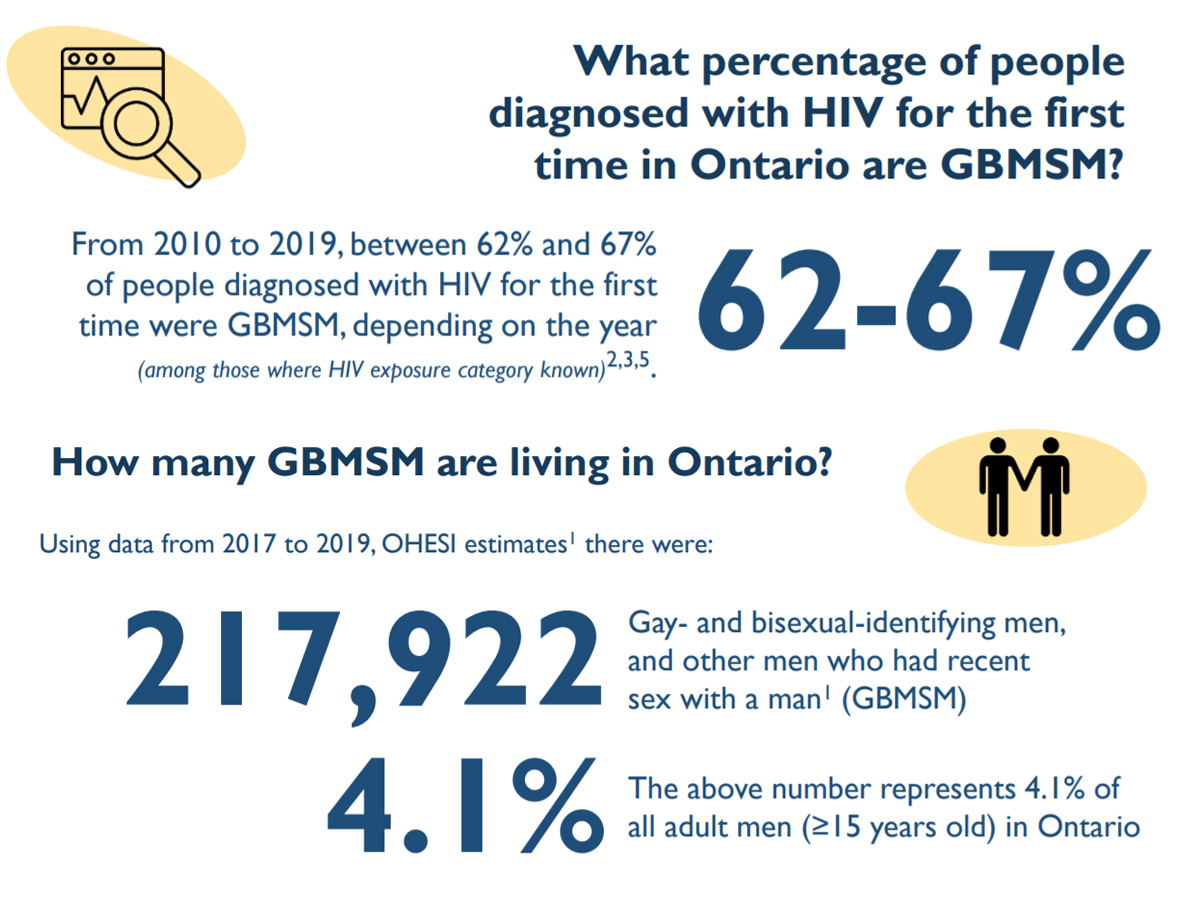
- Looking specifically at first-time HIV diagnoses in 2019, approximately one quarter were among ACB people, whereas OHESI estimates ACB people made up only 4.6% of Ontario’s overall population in 2019.
- More ACB males (70) than females (55) received a first-time HIV diagnosis in 2019, and that pattern has been consistent over time. The majority of ACB men diagnosed for the first time in 2019 (64%) reported male-to-male sexual contact as their risk factor for infection, while most ACB women diagnosed for the first time (85%) reported heterosexual contact with identified risk.
- Once diagnosed with HIV in Ontario, how do ACB people (regardless of whether they already knew their status or are diagnosed for the first time) do on the HIV care cascade (linking to care, being on treatment and being virally suppressed)? Looking at the cascade, in 2015 and 2016, ACB people living with diagnosed HIV were slightly less likely to be in care, on antiretroviral therapy (ART), and virally suppressed than people living with diagnosed HIV overall*. However, in 2017 and 2018, ACB people met levels of these metrics comparable to people living with HIV overall*.
- In 2017, ACB people who were newly diagnosed on average took slightly longer to receive their first viral load test (22 days compared to 17 days) and achieve viral suppression (125 days compared to 119 days), relative to the overall newly diagnosed population.
- Regarding the UNAIDS 90-90-90 targets, we do not have an estimate of the undiagnosed fraction for ACB people living with HIV in Ontario so we cannot ascertain attainment of the full 90-90-90 targets. We have estimated the second and third targets, showing that 83-85% of ACB people diagnosed with HIV in Ontario were on ART in 2018 and 96% of those on ART were virally suppressed, achieving comparable levels of treatment uptake and viral suppression as Ontarians diagnosed with HIV overall.
HIV Diagnoses among ACB people in Ontario
The number of ACB people diagnosed with HIV for the first time has been stable
Of the 229 positive HIV tests in Ontario in 2019 that were among ACB people in Ontario, at least 104 (45.4%) were people who already knew they had HIV – that is, people diagnosed elsewhere who were entering care in Ontario – and 125 (54.6%) are considered first-time HIV diagnoses, meaning HIV acquisition was more likely to have occurred in Ontario. However, due to unreported test history information, OHESI estimates approximately 10% of first-time HIV diagnoses among ACB people had unreported prior knowledge of their HIV status between 2010 and 2019.
Between 2016 and 2019, the number of positive HIV tests from ACB people who already knew their HIV status tripled, while the number of first-time HIV diagnoses was much more stable.
In 2019, ACB people made up about one in every four first-time HIV diagnoses where race/ethnicity and country of birth was reported. This was fairly stable between 2010 and 2019, averaging 24%.
Figure 1. Number of first-time HIV diagnoses and people with previous evidence of HIV among ACB people, 2010-2019

ACB females were more likely than males to have had a previous HIV diagnosis
When we look more closely at the proportion of ACB people who reported already having been diagnosed with HIV, we see that it increased in both males and females between 2014 and 2019, but the increase was greater among females. Over half of ACB females who had a positive HIV test in 2019 already knew their HIV status.
Figure 2. Percent of positive HIV tests with previous evidence of HIV among ACB people, by sex, 2010-2019

More ACB males are diagnosed with HIV for the first time each year than ACB females
In 2019, there were 70 first-time HIV diagnoses among ACB males and 55 among ACB females. The number of first-time HIV diagnoses has been consistently higher among males than females since 2010 (when Ontario first began collecting data on race/ethnicity and country of birth).
Race/ethnicity and country of birth were not reported for 28.5% of all first-time HIV diagnoses between 2010 and 2019. Due to unreported test history information, approximately 8% of first-time HIV diagnoses among ACB males and 14% among ACB females had unreported prior knowledge of their HIV status between 2010 and 2019.
Figure 3. Number of first-time HIV diagnoses among ACB people, by sex, 2010-2019

Large majority of ACB males diagnosed with HIV for the first time report male-to-male sexual contact
Among the first-time HIV diagnoses in ACB males that reported an HIV exposure category in 2019 (66 out of 70), 63.6% reported male-to-male sexual contact, 22.7% reported heterosexual contact with identified risk** and 10.6% reported heterosexual contact with no identified risk. From 2015 to 2019, most ACB males diagnosed with HIV for the first-time reported male-to-male sexual contact.
Figure 4. Percent of first-time HIV diagnoses by HIV exposure category among ACB males, 2015-2019

Heterosexual contact continues to be the only HIV exposure category reported by ACB females
All ACB females diagnosed with HIV for the first time in 2019 reported heterosexual contact as their HIV exposure category. The majority – 85.5% – reported heterosexual sex with someone who had an identified risk** of HIV and 14.5% reported heterosexual sex with someone with no identified risk. This pattern has been consistent over time.
**The “Heterosexual contact, identified risk” category includes diagnoses where sex with a person of the opposite sex/gender is reported and either the individual’s country of birth is reported as an HIV-endemic country, or the individual’s sex partner is reported to be at least one of: HIV-positive; user of injection drugs; born in an HIV-endemic country; a bisexual male.
Nearly two thirds of ACB people diagnosed with HIV for the first time live in Toronto
While most ACB people diagnosed with HIV for the first time live in Toronto, four other regions – Central East, Ottawa, Central West and South West – have ACB populations that are coping with HIV and need culturally competent prevention and care services.
Figure 5. Percent of first-time HIV diagnoses by region among ACB people, 2015-2019

For a much more extensive description of HIV diagnoses among ACB people, Ontarians overall, and each of the other four priority populations, be sure to check out the full report, as well as the supplementary tables.
HIV Care Cascade for ACB People (2015-2018)
The HIV care cascade is a way to assess whether all Ontarians living with HIV are getting appropriate care and have the opportunity to achieve good health outcomes. That cascade monitors three key indicators: the proportion of people diagnosed with HIV who are in care, the proportion on antiretroviral treatment (ART) and the proportion who are virally suppressed (which protects their health and prevents HIV transmission to their sexual partners). We assess that cascade for all people living with diagnosed HIV and by priority population.
To estimate the HIV care cascade for ACB people, we use data on people’s race/ethnicity reported at the time of HIV diagnosis. These data started to be captured in 2009 when the laboratory enhancement form was introduced in Ontario. For more recent diagnoses, ~75% of all diagnoses report race/ethnicity; however, for those diagnosed before 2009, it is not possible to know the race/ethnicity or if a person diagnosed with HIV was ACB.
Overall, cascade indicators improve the longer someone lives with HIV. Therefore, indicators for people diagnosed since 2009 are slightly lower when compared to all people living with diagnosed HIV (as published in the 2018 cascade report). However, in order to provide some understanding of the HIV care cascade for ACB people (only identifiable where diagnosed since 2009), we compare achievement of the HIV care cascade indicators between 2015 and 2018 among ACB people to all people diagnosed in Ontario since 2009. We also describe the latter UNAIDS 90-90-90 targets among ACB people.
Engagement in care has improved since 2015 and is high among ACB people living with HIV
ACB people are as likely as all people diagnosed with HIV to be engaged in care. Between 2015 and 2018, the proportion of ACB people diagnosed since 2009 who were engaged in care increased from 84% to 88%.
Figure 6. Percent of people living with HIV diagnosed after 2009 who are in care, all people vs ACB people, 2015-2018

ACB people living with HIV have high uptake of anti-retroviral treatment
ACB people are as likely as all people diagnosed with HIV to be on anti-retroviral treatment (ART). Between 2015 and 2018, the proportion of ACB people diagnosed since 2009 who were on ART increased from 75% to 83%.
Figure 7. Percent of people living with HIV diagnosed after 2009 who are on anti-retroviral treatment, all people vs ACB people, 2015-2018

Most ACB people living with HIV successfully achieve viral suppression
ACB people are as likely as all people diagnosed with HIV to be virally suppressed. Between 2015 and 2018, the proportion of ACB people diagnosed with HIV who were virally suppressed increased steadily from 71% to 80%.
Figure 8. Percent of people living with HIV diagnosed after 2009 who are virally suppressed, all people vs ACB people, 2015-2018

ACB people living with HIV are improving on the 90-90-90 targets.
Ontario signed on to the UNAIDS 90-90-90 global targets: by 2020, we hoped to have 90% of people with HIV diagnosed, 90% of those diagnosed on treatment and 90% of those on treatment virally suppressed.
While Ontario has made progress towards the UNAIDS 90-90-90 targets since we began measuring them in 2015, we have not yet achieved them. We do not have an estimate of the diagnosed fraction for ACB people living with HIV in Ontario so, instead, we use the overall estimated diagnosed fraction for 2018: 85.2%. However, we do have data on the proportion of ACB people diagnosed with HIV in Ontario who are on treatment and the proportion on treatment who are virally suppressed.
In 2018, we saw that ACB people were doing as well as all people diagnosed with HIV since 2009 on both these measures: 83-85% of ACB with HIV are on treatment and, of those on treatment, 96-97% are virally suppressed. Once ACB people in Ontario are diagnosed and in care and on treatment, they do very well. However, more must be done to ensure we diagnose ACB people living with HIV, engage them in care and support them to stay on treatment.
Figure 9. UNAIDS 90-90-90 targets for ACB people diagnosed after 2009, 2018

*Modelling conducted by the Public Health Agency of Canada on all people living with HIV in Ontario.
ACB people diagnosed with HIV take slightly longer to link to care and become virally suppressed
While ACB people diagnosed with HIV generally do as well as all Ontarians diagnosed with HIV when it comes to being on treatment and virally suppressed, it takes them slightly longer to link to care after their diagnosis. In 2017, the median time after diagnosis to the first viral load test for ACB people newly diagnosed with HIV was 22 days – compared to 17 days for all people newly diagnosed with HIV – and the median time to viral suppression was 125 days – compared to 119 for all people newly diagnosed with HIV.
Notes: Diagnoses attributed to ACB are defined by having indication of being born in an African or Caribbean country and/or Black race/ethnicity. As this information was not reported for 28.5% of all first-time HIV diagnoses and 29.7% of all positive HIV tests between 2010 and 2019, reported counts may represent underestimates. Data shown are where ACB status was reported.*People diagnosed with HIV since 2009.
OHESI is a collaboration involving AIDS and Hepatitis C Programs of the Ontario Ministry of Health, Public Health Ontario, the Public Health Agency of Canada, and the Ontario HIV Treatment Network. The objectives of OHESI are to analyze, monitor and disseminate knowledge products on the epidemiology of HIV in Ontario.
Stay tuned for more OHESI reports coming soon!