The Ontario HIV Epidemiology and Surveillance Initiative (OHESI) is pleased to announce the release of a new report titled “HIV Testing in Ontario, 2019”.
A robust HIV testing program ensures that individuals at risk receive regular HIV tests and that people who are living with HIV can learn their status and be linked to care. HIV testing is also an important gateway to prevention services for people who test HIV-negative. Understanding trends in HIV testing can also help Ontario measure the success of its HIV testing initiatives.
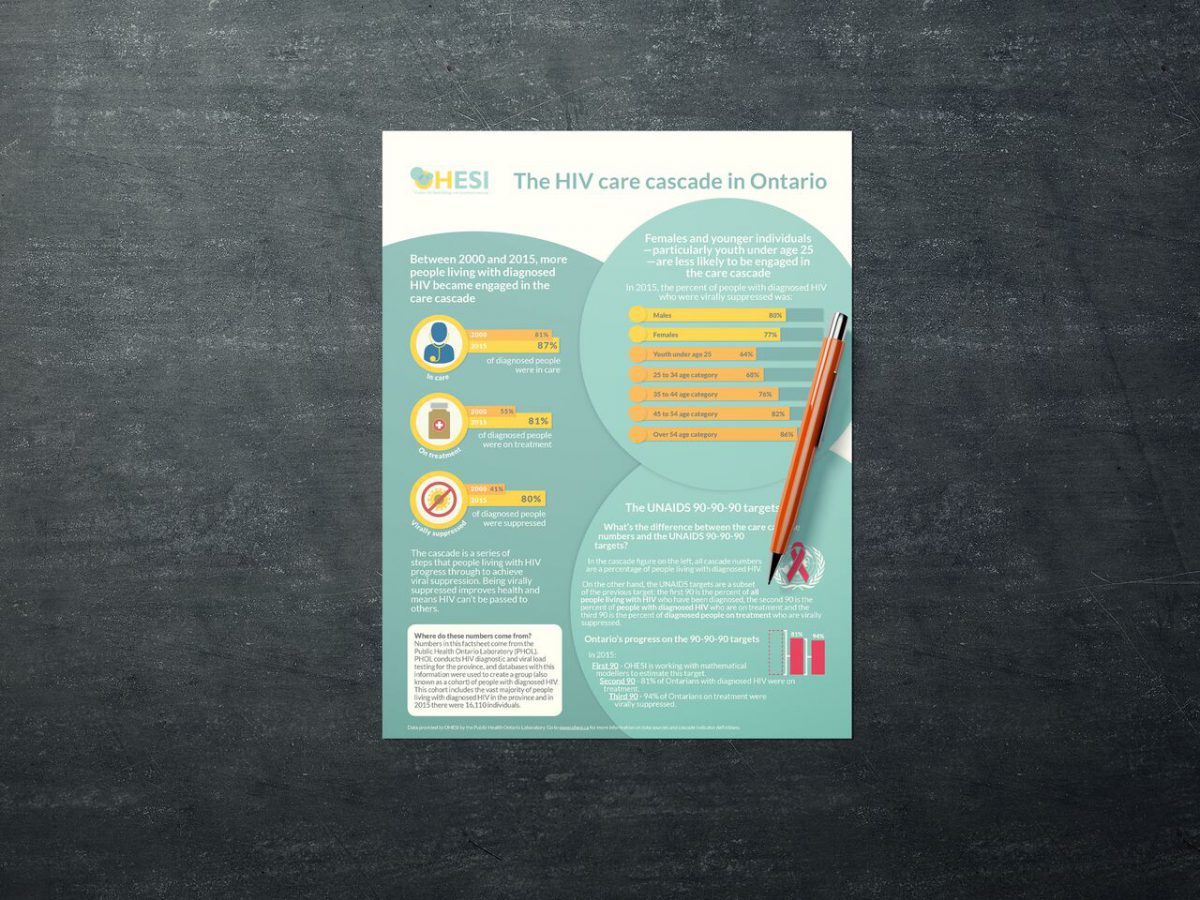
In the 2019 HIV Testing Report, OHESI describes the trends in HIV testing in Ontario over the past decade (2010-2019), with a focus on HIV tests in 2019. The report includes analyses broken down by type of test (nominal, coded, and anonymous), sex, age, HIV exposure category, and geographic location (health regions), as well as information specific to rapid/point-of-care (POC) and prenatal HIV testing. New to this report are analysis by HIV test submitter type and by transgender identity and race/ethnicity (based on the new HIV test requisition implemented in 2018). Metrics described in the report include the number and percent of HIV tests, rates of HIV tests per 1,000 people, and HIV test positivity rates (i.e. the percentage of HIV diagnostic tests with a confirmed HIV-positive result).
Some key findings:
- In 2019, 677,251 HIV tests were conducted in Ontario – equivalent to an HIV testing rate of 46.6 tests per 1,000 people. Of note, negative prenatal HIV tests were analyzed separately in this report.
- While the number of tests conducted remained relatively stable between 2010 and 2013, it increased 53.3% between 2013 and 2019. The HIV testing rate per 1,000 people also increased 42.4% during this time.
- In 2019, the number of HIV tests was slightly greater among males (333,521) than females (325,317). Only in 2017 and 2019 was the number of HIV tests among males greater than among females.
- While the HIV test positivity rate decreased over time for both sexes, it was consistently three to five times higher among males than females. In 2019, the HIV test positivity rate was 0.15% for males and 0.05% for females.
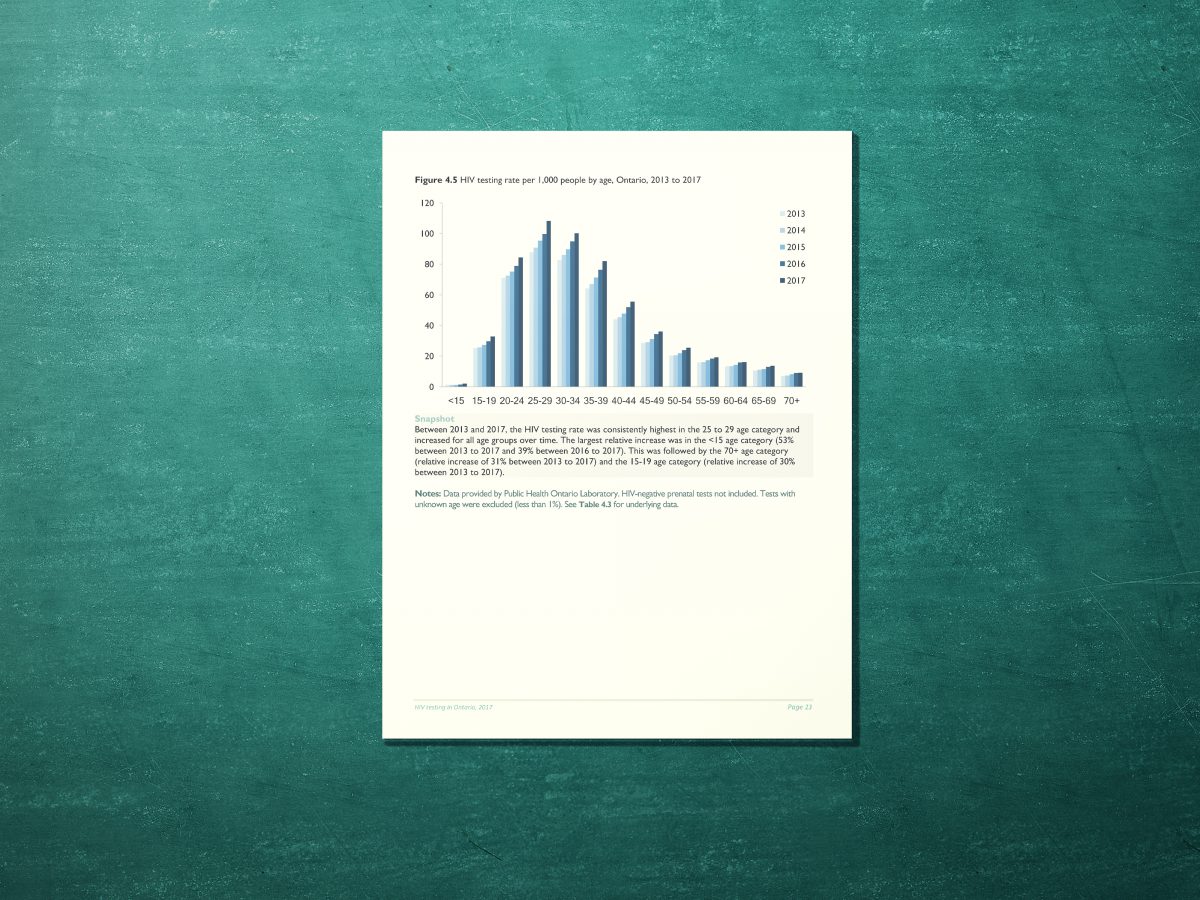
- Between 2015 and 2019, the HIV testing rate per 1,000 people increased for all age groups by an average of 34% and was consistently highest in the 25 to 29 age category.
- The HIV test positivity rate in 2019 was highest in the 55-59 age category for both males (0.26%) and females (0.09%); however, people testing in this age category tested at a lower rate and had a relatively lower number of positive tests.
- In 2019, the vast majority of HIV tests (96.3%) were nominal and the remainder were coded (1.2%) or anonymous (2.4%).
- While the HIV test positivity rate has decreased over time for all test types, it was consistently at least four times higher among people who tested anonymously than those who tested nominally. In 2019, the HIV test positivity rate was 0.09% for nominal testing, 0.14% for coded testing and 0.48% for anonymous testing.
- Between 2015 and 2019, the proportion of HIV tests in males attributed to men who have sex with men (MSM) increased from 10.8% to 13.1%. Approximately 63% of HIV tests among males had unknown exposure category.
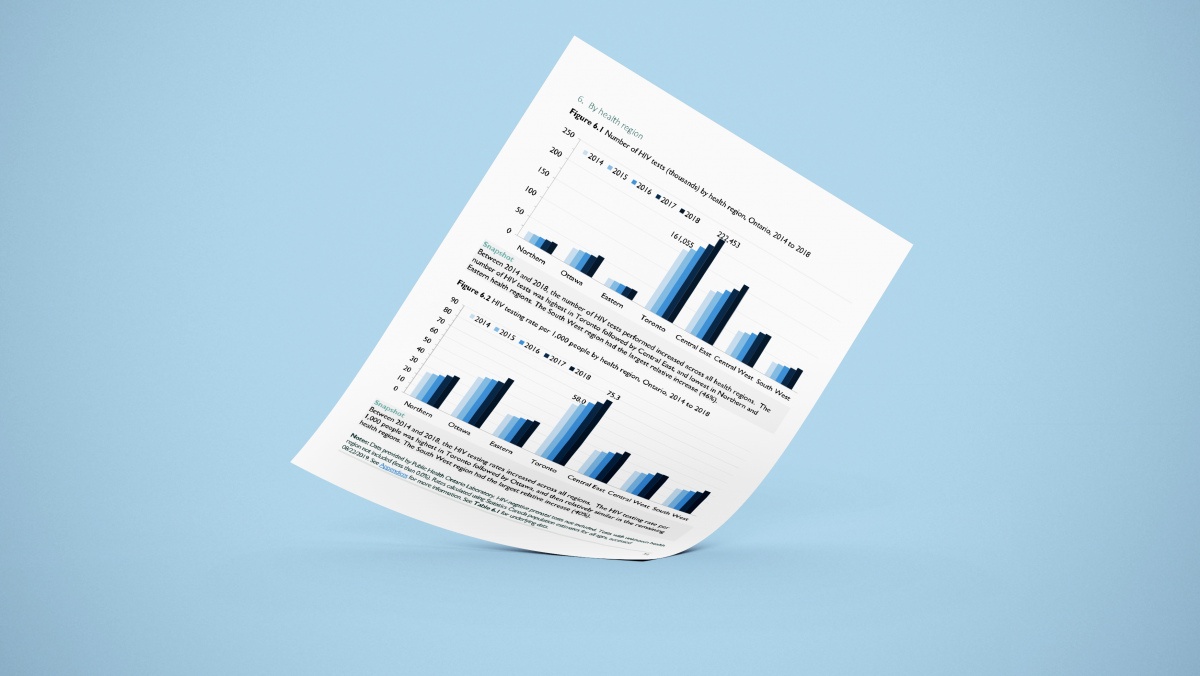
- In 2019, the HIV testing rate per 1,000 people was highest in Toronto (80.0) followed by Ottawa (53.0). In the other five health regions, the HIV testing rate ranged from 31.4 (Eastern) to 40.2 (Central East). The number of HIV tests and the HIV testing rate per 1,000 people increased between 2018 and 2019 in all health regions, with the exception of the South West region.
- In 2019, HIV tests submitted by “other physicians/clinics/labs” comprised the largest proportion of HIV tests (44.2%), followed by immigration physicians/clinics (14.1%) and HIV treating physicians/clinics (11.5%).
- In 2019, the largest number of positive results among males were submitted by “other physicians/clinics/labs” (140, 27.2%), and among females were submitted by immigration physicians/clinics (53, 31.4%).
- In 2019, of the 223,198 HIV tests submitted via the new test requisition with known sex, 178 (0.08%) were among transgender females, and 114 (0.05%) were among transgender males.
- In 2019, among the 226,716 HIV tests submitted via the new HIV test requisition, the largest proportion of HIV tests was among White individuals (29.3%), followed by Black (5.8%), East/Southeast Asian (4.9%), and South Asian (3.6%) individuals. Approximately half (49.7%) of these tests had unknown or missing race/ethnicity information.
- Between 2014 and 2019, the number of point-of-care (POC) tests decreased from 30,117 to 19,414 tests, while the POC HIV test positivity rate fluctuated between 0.42% (2015) and 0.69% (2018) before decreasing to a low of 0.32% in 2019.
- In 2019, the vast majority of HIV tests (97.1%) were standard, laboratory tests and the remainder were POC (2.9%); the majority of POC tests are provided anonymously.
- Between 2012 and 2019, the estimated proportion of all pregnant people who received a prenatal HIV test increased from 94.2% to 97.4%.
Stay tuned for future reports from OHESI!
L’Initiative d’Épidémiologie et de Surveillance du VIH en Ontario (OHESI) a le plaisir d’annoncer la publication d’un nouveau rapport intitulé “2019, le dépistage du VIH en Ontario“.
Un solide programme de dépistage du VIH permet de s’assurer que les personnes à risque subissent régulièrement des tests de dépistage du VIH et que les personnes qui vivent avec le VIH puissent connaître leur statut et soient arrimer aux soins. Le dépistage du VIH est également une passerelle importante vers les services de prévention pour les personnes dont le test est négatif. La compréhension des tendances en matière de dépistage du VIH peut également aider l’Ontario à mesurer le succès de ses initiatives de dépistage du VIH.
Dans le rapport 2019 sur le dépistage du VIH, l’OHESI décrit les tendances du dépistage du VIH en Ontario au cours de la dernière décennie (2010-2019), en mettant l’accent sur les tests de dépistage du VIH en 2019. Le rapport comprend des analyses ventilées selon le type de test (nominal, codé et anonyme), le sexe, l’âge, la catégorie d’exposition au VIH et l’emplacement géographique (régions sanitaires), ainsi que des informations spécifiques au dépistage rapide/point de service (PS) et au dépistage prénatal du VIH. Les nouveautés de ce rapport se situent au niveau des analyses par type de personne ayant soumis le test VIH et par identité transgenre et race/origine ethnique (sur la base de la nouvelle demande de test de dépistage du VIH mise en œuvre en 2018). Les métriques décrites dans le rapport comprennent le nombre et le pourcentage des tests de dépistage du VIH, les taux sur 1 000 personnes et les taux de positivité des tests de dépistage du VIH (c’est-à-dire le pourcentage des tests diagnostiques du VIH avec un résultat positif confirmé).
Quelques principales conclusions :
- En 2019, 677 251 tests de dépistage du VIH ont été effectués en Ontario – ce qui équivaut à un taux de dépistage du VIH de 46,6 tests sur 1 000 personnes. Il convient de noter que les tests de dépistage du VIH prénataux négatifs ont été analysés séparément dans ce rapport.
- Bien que le nombre de tests effectués soit resté relativement stable entre 2010 et 2013, il a augmenté de 53,3 % entre 2013 et 2019. Le taux de dépistage du VIH sur 1 000 personnes a également augmenté de 42,4 % au cours de cette période.
- En 2019, le nombre de tests de dépistage du VIH était légèrement supérieur chez les hommes (333 521) que chez les femmes (325 317). Ce n’est qu’en 2017 et 2019 que le nombre de tests de dépistage du VIH chez les hommes était supérieur à celui des femmes.
- Bien que le taux de positivité des tests de dépistage du VIH ait diminué au fil du temps pour les deux sexes, il était constamment de trois à cinq fois plus élevé chez les hommes que chez les femmes. En 2019, le taux de positivité des tests de dépistage du VIH était de 0,15% chez les hommes et de 0,05% chez les femmes.
- Entre 2015 et 2019, le taux de dépistage du VIH sur 1 000 personnes a augmenté pour tous les groupes d’âge de 34 % en moyenne et était systématiquement plus élevé dans la catégorie des 25 à 29 ans.
- En 2019, le taux de positivité des tests de dépistage du VIH était le plus élevé dans la catégorie d’âge des 55 à 59 ans, tant pour les hommes (0,26 %) que pour les femmes (0,09 %) ; toutefois, les personnes testées dans cette catégorie d’âge l’ont été à un taux plus faible et ont eu un nombre relativement plus faible de tests positifs.
- En 2019, la grande majorité des tests de dépistage du VIH (96,3 %) étaient nominatifs et les autres étaient codés (1,2 %) ou anonymes (2,4 %).
- Bien que le taux de positivité des tests de dépistage du VIH ait diminué au fil du temps pour tous les types de tests, il a toujours été au moins quatre fois plus élevé chez les personnes ayant effectué un test anonyme que chez celles ayant effectué un test nominal. En 2019, le taux de positivité des tests de dépistage du VIH était de 0,09 % pour les tests nominaux, de 0,14 % pour les tests codés et de 0,48 % pour les tests anonymes.
- Entre 2015 et 2019, la proportion des tests de dépistage du VIH chez les hommes attribués aux hommes ayant des relations sexuelles avec des hommes (HSH) a augmenté de 10,8% à 13,1%. Environ 63 % des tests de dépistage du VIH chez les hommes avaient une catégorie d’exposition inconnue.
- En 2019, le taux de dépistage du VIH sur 1 000 personnes était le plus élevé à Toronto (80,0 %), suivi d’Ottawa (53,0 %). Dans les cinq autres régions sanitaires, le taux de dépistage du VIH variait de 31,4 % (Est) à 40,2 % (Centre-Est). Le nombre des tests de dépistage du VIH et le taux de dépistage du VIH sur 1 000 personnes ont augmenté entre 2018 et 2019 dans toutes les régions sanitaires, à l’exception de la région du Sud-Ouest.
- En 2019, les tests de dépistage du VIH soumis par les “autres médecins/cliniques/laboratoires” représentaient la plus grande proportion de tests de dépistage du VIH (44,2 %), suivis par les médecins/cliniques de l’immigration (14,1 %) et les médecins/cliniques traitant le VIH (11,5 %).
- En 2019, le plus grand nombre de résultats positifs chez les hommes a été soumis par les “autres médecins/cliniques/laboratoires” (140 soit 27,2 %), et chez les femmes par les médecins/cliniques de l’immigration (53 soit 31,4 %).
- En 2019, parmi les 223 198 tests de dépistage du VIH soumis via la nouvelle demande de test avec le sexe connu, 178 (0,08 %) concernaient des femmes transgenres et 114 (0,05 %) des hommes transgenres.
- En 2019, parmi les 226 716 tests de dépistage du VIH soumis dans le cadre de la nouvelle demande de test du VIH, la plus grande proportion de tests de dépistage du VIH concernait les Blancs (29,3 %), suivis par les Noirs (5,8 %), les Asiatiques de l’Est/Sud-Est (4,9 %) et les Asiatiques du Sud (3,6 %). Environ la moitié (49,7 %) de ces tests comportaient des informations sur la race ou l’origine ethnique inconnues ou manquantes.
- Entre 2014 et 2019, le nombre de tests au point de service (PS) a diminué, passant de 30 117 à 19 414 tests, tandis que le taux de positivité des tests de dépistage du VIH au PS a fluctué entre 0,42 % (2015) et 0,69 % (2018) avant de baisser à un faible taux de 0,32 % en 2019.
- En 2019, la grande majorité des tests de dépistage du VIH (97,1 %) étaient des tests de laboratoire standard, le reste étant des tests des PS (2,9 %) ; la majorité des tests des PS sont fournis de façon anonyme.
- Entre 2012 et 2019, la proportion estimée de toutes les personnes enceintes ayant bénéficié d’un test prénatal de dépistage du VIH est passée de 94,2 % à 97,4 %.
Restez à l’écoute des prochains rapports de l’OHESI !