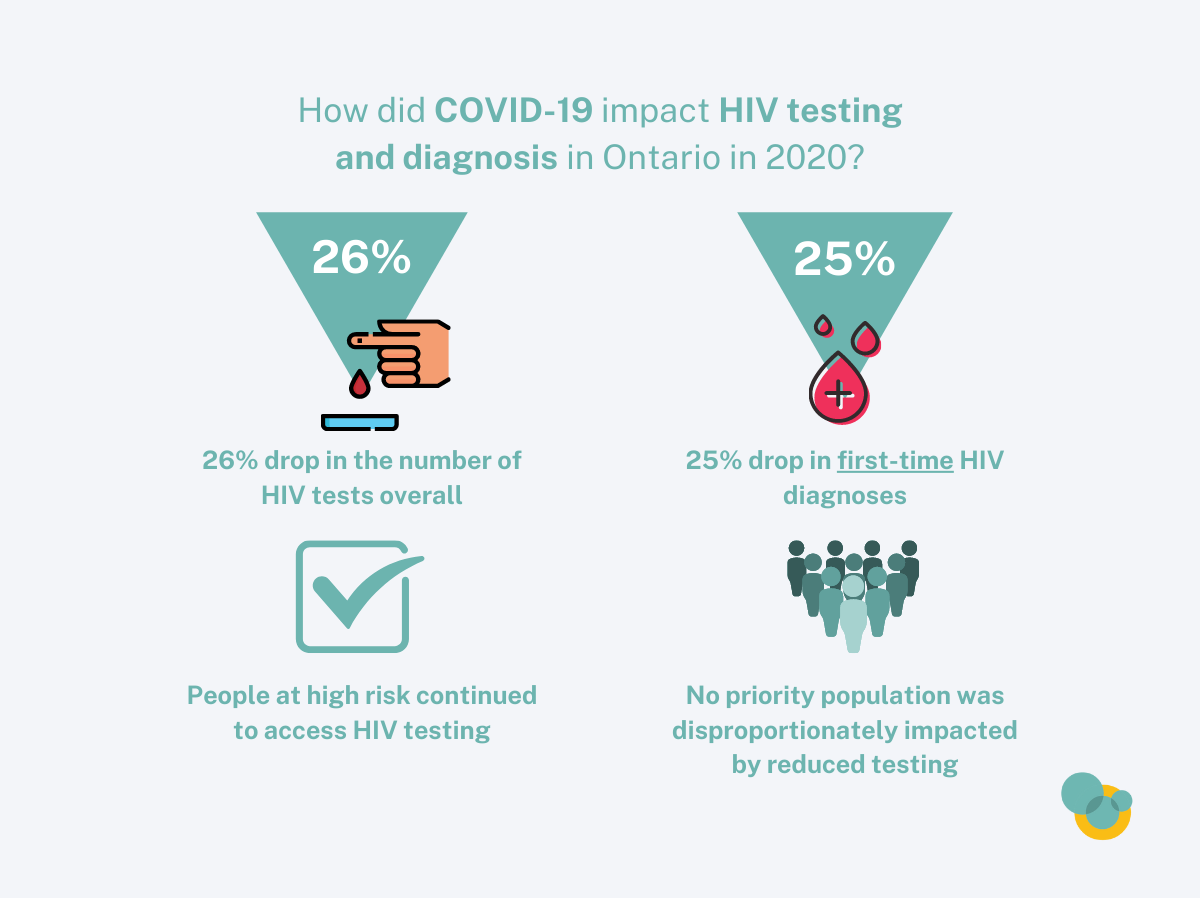
The COVID-19 pandemic has disrupted access to health services, including HIV testing and clinical care. The impact of COVID-19 on HIV testing, diagnoses, and surveillance data obscures trends and makes it difficult to interpret the current state of Ontario’s HIV epidemic.
In 2020, we saw a:
- 26% drop in the number of HIV tests overall (from 677,254 in 2019 to 500,517 in 2020)
- 39% drop in positive tests with previous evidence of HIV[1] (from 239 to 146) – likely due to decreases in migration during the pandemic (fewer people moving into the province)
- 25% drop in first-time HIV diagnoses[2] (from 683 to 515) likely due to a combination of: missed diagnoses, a real drop in new infections (less HIV transmission), and decreases in migration.[3]
Number of HIV Tests Down in Males and Females in 2020
This decline in the number of HIV diagnostic tests was a reversal of the trend of increasing tests over the past decade.
Figure 1: HIV diagnostic tests, by sex and year, Ontario

Both First-time HIV Diagnoses and Persons with Previous Evidence of HIV Down in 2020
The number of both first-time diagnoses and positive tests with previous evidence of HIV decreased substantially in 2020.
Figure 2: First-time HIV diagnoses and persons with previous evidence of HIV, by year, Ontario

The number of tests with previous evidence of HIV decreased for the first time since 2012. This decrease is likely due to a decrease in migration: fewer people moving to Ontario and being tested for the first time in the province due to the pandemic.
The decrease in first-time HIV diagnoses is likely due to three contributors:
- Some missed diagnoses because of the drop in testing. Some people may have not been diagnosed because they did not access testing, when they would have under normal (i.e. non-COVID) circumstances.
- A real decrease in HIV transmission. Ontario saw a drop in first-time diagnoses in 2019, With more people with HIV being virally suppressed and more people on PrEP, part of the decrease in 2020 may be due to less local transmission, especially among some groups of gay, bisexual and other men who have sex with men (GBMSM). Restrictions caused by the COVID-19 pandemic also likely reduced transmission of HIV.
- The decrease in migration. Each year, some people with previous evidence of HIV are misclassified as first-time diagnoses because of missing information on their test history. With decreased migration in 2020, there were a smaller number of these misclassified first-time HIV diagnoses, thereby contributing to a lower number of first-time HIV diagnoses overall.
People at High Risk Continued to Access Testing in 2020
Over the past decade, we had seen a steady drop in the HIV test positivity rate among males. In 2020, despite the 29% drop in HIV tests in males, the positivity rate among males increased. That means that males at high risk were still accessing testing. Testing may also have been more targeted to those at elevated risk or with symptoms.
Figure 3: HIV test positivity, by sex and year, Ontario

It appears that no particular priority population was disproportionately impacted by reduced HIV testing
During 2020, a significant number of HIV test requisition forms and follow-up reports were not fully completed. As a result, we are missing some information that helps us understand HIV transmission trends in populations, including HIV test history, HIV risk factors and race/ethnicity.
Priority populations are not mutually exclusive and therefore a diagnosis from a single individual can be assigned to more than one priority population. The percentage of first-time diagnoses that could not be assigned to a priority population due to missing information doubled in 2020: from 14.5% to 28.3%. However, when we examine first-time diagnoses that could be assigned, we see little change in the distribution of diagnoses between 2020 and 2019. Gay, bisexual, and other men who have sex with men (GBMSM) continued to account for >60% of first-time diagnoses, and the decrease in the percentage of first-time HIV diagnoses attributed to African, Caribbean and Black (ACB) people, people who inject drugs (PWID), and Women in 2020 are within 5-year trends. In addition, ACB people and Women are more likely than other priority populations to have a previous HIV diagnosis at the time of their first HIV test in Ontario. This means that whereas in previous years, numbers of first-time HIV diagnoses in these priority populations were slightly inflated by misclassified first-time HIV diagnoses, the reduced migration in 2020 has reduced this element of inflation particularly for these two populations.
Figure 4: First-time HIV diagnoses by priority population, comparing 2019 to 2020, Ontario

To fully understand the impact of the COVID-19 pandemic on HIV testing, diagnoses and treatment – including where diagnoses might have been missed – we will have to look more closely at the 2020 data and ongoing surveillance information and will provide further insight in the yearly diagnoses and testing surveillance reports.
[1] People who already knew their HIV status at the time of a first HIV test in Ontario (i.e. people moving to Ontario)
[2] People receiving an HIV diagnosis for the first time
[3] Each year, some people with previous evidence of HIV are misclassified as first-time diagnoses because of missing information on their test history.